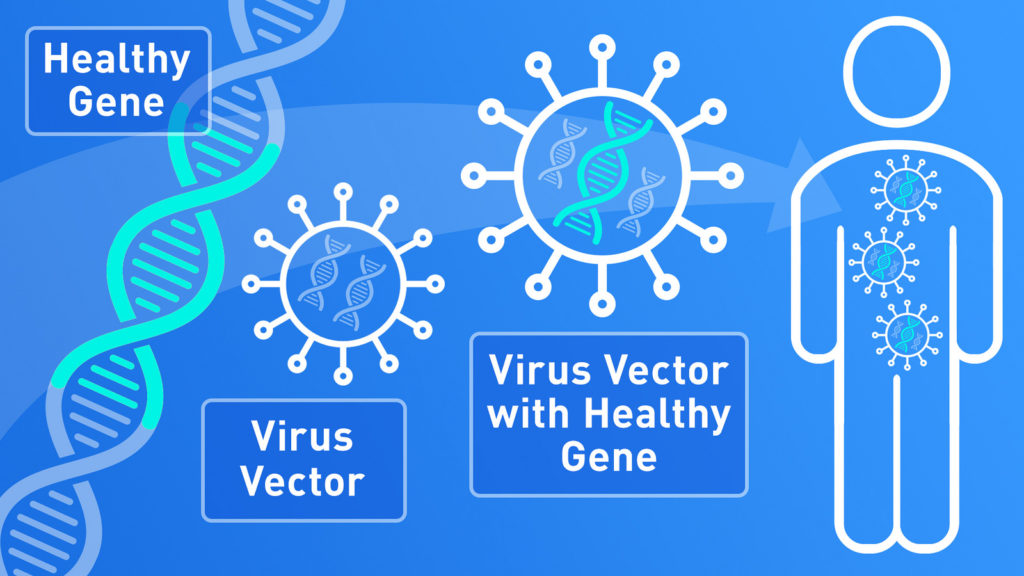
New approaches for preventing and treating illnesses are on the rise, including the use of gene therapy through vaccines. With this technique, healthy copies of genes can be introduced to the body to reverse the bad effects of genes working incorrectly. This form of treatment would be especially helpful for genetic disorders, whose problems are based in our DNA. However, a major obstacle in this treatment is the delivery system of the new genes. That is, how do we bring the healthy genes into our cells and have them turn on in the first place?
So far, viruses have proven to be a major help as a gene-delivery system. The nature of viruses is to copy themselves over and over, so they’re an excellent way to spread a desired gene within the body. Of course, they’re modified first so they can’t cause illness. In this study, researchers at Uppsala University in Sweden used a modified tick-borne encephalitis virus (TBEV) to test whether a smaller and edited version of the virus would be able to copy itself well in cells. Through this study, researchers are hoping to get closer to creating gene-based vaccines.
This encephalitis virus belongs to a category of viruses called flavivirus, which includes others like Zika virus, West Nile virus, and Dengue virus. Flaviviruses are often studied as a delivery system because it’s easy to change their structure and contents. Unlike other viruses, this type of virus doesn’t change the host DNA. Lastly, the natural way flaviviruses infect people is through the skin, which means they’d be effective at entering skin cells through a vaccine
For this experiment, researchers grew hamster cells and monkey cells in a lab in order to inject them with the modified virus. Four versions of the virus were made to test how well each version worked. The animal cells were then injected with one of them and placed in a heated room for 96 hours. The researchers collected samples from the test cells for analysis three times—after 24 hours, 48 hours, and 96 hours.
For each time point, researchers looked at the samples to find out the amount of virus production. They had to mix in markers that would latch onto the virus and then light up in a special gel, allowing the researchers to get a sense of how well the virus was multiplying. A darker mark in the gel generally meant there was more virus present in that sample. After 24 hours, no marks appeared in the gel. However, marks later appeared at the 48-hour and 96-hour time points. The marks at the 96-hour period were also darker than the 48-hour period, meaning that even more of the virus had been produced at a steady rate during that time. One version of the modified virus appeared to be more effective than the others, but all versions produced some level of success.
Scientists also looked at the animal cells under a microscope to see where the virus went in the cells. They found that not only did the virus appear inside the cell, but it managed to use ways to exit the cells naturally, which would ultimately help the virus spread helpful genes if used in gene therapy.
The researchers concluded that their modified versions of the virus were indeed safe and effective for surviving and multiplying in host cells. The natural life cycle of the virus provides a steady rate of replication and spreading, which would help deliver gene therapy efficiently. Thus, further research can build upon this discovery and help design vaccines in the future to deliver healthy genes to human bodies.