Cells, the basic unit of the human body, are largely made of molecules known as proteins. Cells create proteins from building blocks called amino acids based on blueprints found in their genetic material, or DNA. When these DNA blueprints become damaged, the cells start using the wrong amino acids to create proteins. This is known as a missense mutation. Missense mutations can cause the cells of a person’s body to grow out of control and become a cancerous tumor.
Currently, doctors extract microscopic tissue samples, like the lung or spleen, from patients diagnosed with cancer to learn about their specific tumor type directly from the DNA. (This is different from “staging,” or how advanced a tumor is.) Tumors have unique gene sequences, and knowing them is helpful for determining the best treatment. Although these procedures are invasive and painful, attempts to replace them with blood tests that can detect tumor DNA have failed because tumor cells don’t typically release enough DNA into the bloodstream to be detected. Researchers would like to improve the sensitivity of these tests to replace more invasive procedures.
A group of scientists recently conducted a cancer study at the St. Petersburg City Cancer Center in Russia which might help answer this question. Dr. Ekaterina Kuligina and her colleagues hypothesized that subjecting rectal cancer patients to standard radiation therapy could increase cancer cell DNA in their blood to detectable levels. The answer would bring the medical field one step closer to determining if it can use blood samples, rather than tissue extractions, to accurately and non-intrusively gain the sort of information on cancer patients’ tumors necessary for them to receive individualized treatments.
The research team predicted that giving standard radiation treatments would work by forcing cancer cells to release their DNA, called “ctDNA,” upon dying from radiation exposure. Because ctDNA testing lacked sensitivity, previous work had only found minor uses for it, such as examining emerging tumor mutations responsible for drug resistance. The innovation in this study involved finding a way to increase ctDNA to detectable levels so it could be used to directly determine the potential effectiveness of different treatments and the degree to which cancer returned in relapsed patients.
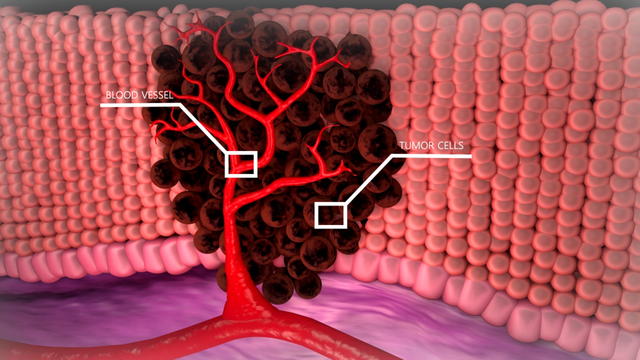
An artists rendering of a tumor surrounding blood vessels. When the tumor is exposed to radiation, its cells break apart, releasing tumor DNA into the blood. This can be collected for analysis, to more precisely determine the cancer’s genome. Source: Wikimedia commons
They recruited a group of 9 rectal cancer patients because radiation therapy is the traditional treatment for them. Also, cancerous missense mutations are common in this cancer type. The scientists carried out their experiment by treating each patient with standard radiation therapy, which was delivered in several doses. In order to see whether the radiation therapy changed the patients’ ctDNA blood content, the team took 11 blood samples from each patient – 1 an hour before radiation and 10 more at regular intervals after radiation. Then, they used a procedure called PCR to “read” the collected DNA and determine the specific type of mutations the patient’s cancer had.
The results of the experiment supported the research team’s prediction. At its start, less than 50% of the rectal cancer patients had enough ctDNA in their bloodstream for their cancer to be detected by blood testing alone. After they had been treated with radiation therapy, the share of patients whose ctDNA content reached levels that could be picked up by blood tests increased by 50%. Almost all of the patients with detectable levels of ctDNA prior to the experiment experienced substantial increases, by as much as 5 times their pre-treatment levels.
The researchers suggest that future studies should measure how ctDNA levels naturally fluctuate within patients’ bloodstreams. They wondered if other patient groups, such as those suffering from lung cancer, could receive similar benefits from radiation therapy.
Because of this study, we now have evidence that blood sampling with standard radiation treatment might be able to replace tissue extraction as a way to give doctors the data they need to target each patients’ unique cancers with tailored therapies.
While use of radiation therapy to damage cancerous growths in patients can still pose a danger if care isn’t taken to avoid irradiating nearby veins or arteries, these concerns are outweighed by the benefits that blood testing can provide in terms of reduced intrusiveness and increased treatment accuracy. Some future uses could be identifying the procedures appropriate for patients’ tumors, assessing how well a given treatmentant plan is working, or observing how severely a patient’s cancer has returned.


