Personalized cancer treatment is on the rise. Cancer is not just one disease but thousands of different types and subtypes that each respond to treatment a little differently. Doctors are able to do their jobs best when they have a way to predict who will respond to a given treatment a certain way.
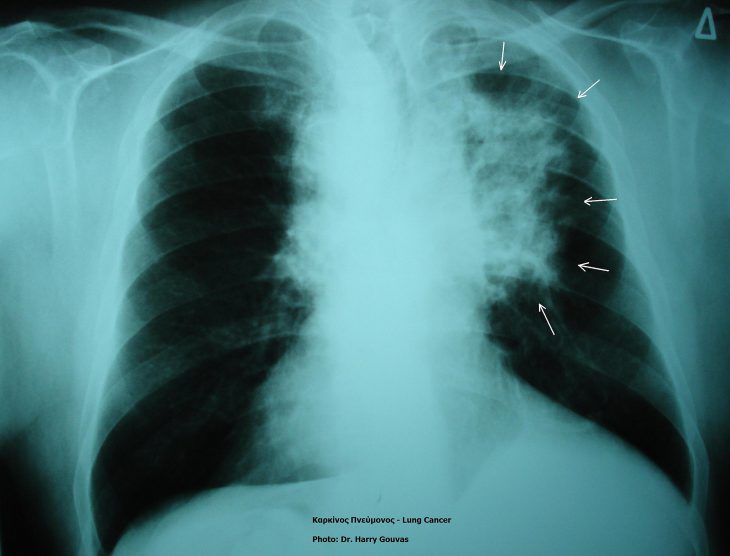
Researchers are looking for techniques that can predict how well a tumor will respond to a treatment. One way to do this is by measuring “biomarkers.” Biomarkers for cancer are “signals” that a tumor has a certain trait that might make it susceptible to a medication or procedure. Non-small cell lung cancer is the most common type of lung cancer found.
In order to suppress the immune system, some tumors produce a molecule called PD-L1. One of the main treatments for non-small cell lung cancer is called an immune checkpoint inhibitor, which addresses this problem. Immune checkpoint inhibitors are medications that block PD-L1, stimulating an immune response against the tumor.
However, immune checkpoint inhibitor therapy does not benefit all patients affected by non-small cell lung cancer. A multi-institution team of scientists tried to use a certain type of DNA change, called a frameshift mutation, to help predict which patients will respond to immune checkpoint inhibitors.
Frameshift mutations are when parts of the gene sequence are deleted or added, so the cell might produce altered versions of its usual proteins. These weird proteins result from frameshift mutations in the tumor and can be detected by doctors using the method of tumor biopsy to find biomarkers. The proteins are made detectable by the patient’s immune system by marking the tumor as an enemy cell. If the tumor expresses the marked proteins, they may also respond better to the checkpoint inhibitor drugs.
To answer their questions, they first searched a database of cancer clinical samples of copied DNA sequences for an RNA molecule, called the Cancer Genome Atlas, for two types of lung cancers: adenocarcinoma and squamous cell carcinoma. The transcriptional expression data was split into four groups depending on how common frameshift mutations were found: low, medium-low, medium-high, or high. If their hypothesis is accurate, they would expect to see a stronger immune system attack on tumors with more frameshift mutations.
Researchers observed that in both lung adenocarcinoma as well as squamous cell lung carcinoma, the group with the highest number of frameshift mutations in the tumor had more immune cells present in the tumor. With more frameshift mutations, the immune response against the tumors was more pronounced and easier to objectively measure the attacking tumors. But, these patients did not necessarily survive longer.
Researchers divided the non-small cell lung cancer patient data into two groups, those with and without frameshift mutations. Then they compared patients based on how long they were on the treatment before their tumor started to grow again.
The frameshift mutation group had a longer time period before progression and stayed in treatment on average 6.2 months, while the non-mutation group stayed in treatment an average of 2.7 months. Their overall survival rate was followed over time, and there was no statistically significant difference between the low and high frameshift mutations. The “low” group survived an average of 16 months and the “high” group survived an average of 10 months. With fewer frameshift mutations, there was a difference in time until the tumor grew again, but there was not a difference in the total survival time.
In patients with more frameshift mutations, the treatment activated a stronger immune response, and their tumors grew more slowly. This was seen in the patients with and without the frameshift mutations and the overall survival rate observed over time was not much different from the progression-free survival rate.
The Cancer Genome Atlas did not actually contain a large number of patients who were treated with checkpoint inhibitor drugs, which limited what can be learned from this study. A larger study with more checkpoint inhibitor patients would help. Researchers also were observing RNA and it showed there was not enough evidence of frameshift mutations to conclude how these drugs can alter the testing of frameshift mutations in DNA. Also, they could not compare frameshift mutations and the more popular biomarker used, PD-L1, due to the amount of data available on PD-L1. They recommend that treatments in the future should be determined based on multiple biomarkers rather than just one.