People with lung and airway diseases are at high risk of developing bacterial infections, especially if they need a ventilator. Antibiotics can treat these infections, but increasing antibiotic resistance threatens to reduce treatment options. Scientists are working to develop new antibiotics and therapies that can kill antibiotic-resistant bacteria.
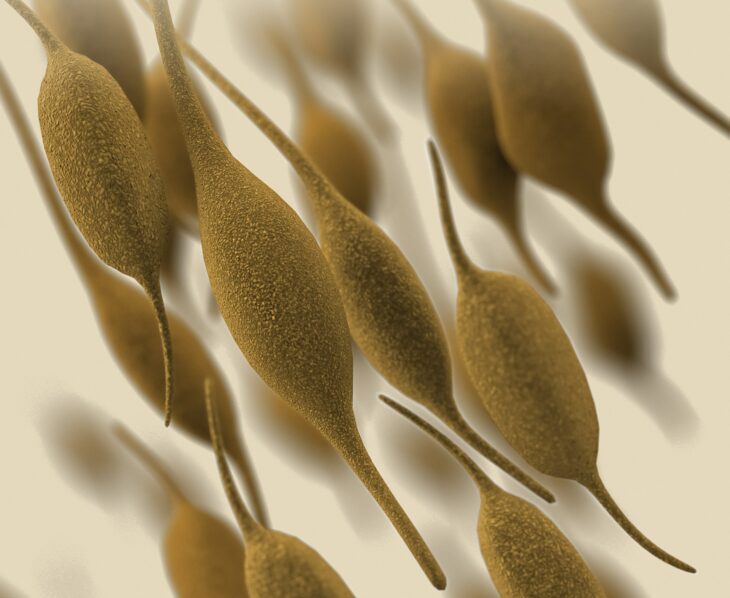
Many bacteria can protect themselves from antibiotics by clustering together and releasing a sticky substance containing sugars and proteins that help them to attach to surfaces. These layers of bacteria are called biofilms, and they can cause serious respiratory infections when they form on ventilators.
Researchers in Barcelona have developed a new type of therapy to target a species of antibiotic-resistant bacteria called Pseudomonas aeruginosa, which forms biofilms and causes lung infections. The scientists engineered another species of bacteria, called Mycoplasma pneumoniae, to fight P. aeruginosa biofilms.
M. pneumoniae can also cause lung infections, so the authors began by creating a weak version of the bacteria that could safely be used in the lungs. They did this by altering the DNA of M. pneumoniae to remove genes that cause lung damage. The researchers wanted the bacteria to live long enough to fight P. aeruginosa infections, so they were careful not to disrupt any genes the bacteria use to survive in the lungs. They tested the safety of the weakened M. pneumoniae in mice, and showed it caused minimal lung damage and inflammation after 4 days in the lungs.
After this, the authors introduced new genes the M. pneumoniae could use to break up biofilms and fight P. aeruginosa. Given the right conditions, many bacteria can take up DNA from the environment around them and use it like their own. This process is called transformation, and is used by microbiologists to feed DNA to bacteria and change their behavior. The team used transformation to deliver 3 genes M. pneumoniae could use to make enzymes that break up the sugars in biofilms. They also added a gene for a protein called pyocin L1, which is a type of antibiotic that doesn’t harm M. pneumoniae but can kill P. aeruginosa.
Next, the authors checked whether the modified M. pneumoniae could break down P. aeruginosa biofilms using their new genes. They added the modified M. pneumoniae to biofilms grown on a plate and waited 4 hours. Then they washed out the plate and added a dye that stains biofilms, called Crystal Violet. If the biofilm on the plate was still intact, it would be stained purple by the Crystal Violet, but if it was broken down by the M. pneumoniae it would be washed away.
Using this technique, the team found the modified M. pneumoniae destroyed more biofilms than the standard M. pneumoniae. The authors also showed the modified M. pneumoniae could dissolve biofilms growing on discarded ventilator tubes from hospitalized patients.
The authors next investigated whether the modified M. pneumoniae could kill the strains of P. aeruginosa within biofilms. They found the modified M. pneumoniae could stop 3 P. aeruginosa strains from growing, but failed against 1 strain.
They engineered another modified M. pneumoniae by adding the gene of an antibiotic protein called pyocin S5 instead of pyocin L1. This new modified bacterium halted the growth of the final P. aeruginosa strain. The authors stated this showed the level of flexibility of the modified M. pneumoniae as a therapy for treating unwanted biofilms.
The team then tested M. pneumoniae as a treatment for mice infected with P. aeruginosa. They found mice treated with the modified M. pneumoniae cleared the infection in 26 hours. The treated mice also lived longer and had less lung damage than untreated mice.
By arming M. pneumoniae with genes to break down biofilms and fight P. aeruginosa, the authors concluded this therapy could potentially treat respiratory infections. The authors also highlighted that engineered bacteria could be adapted to deliver therapy for other types of lung diseases in the future. However, as this study was carried out using mice, more research will be needed to translate it into human medicine.