How does COVID-19 affect patients with cancer? New research performed using data from hospitals in Hubei Province, China suggest that cancer patients are more likely to be harmed by SARS-CoV-2 than those who do not have cancer. This is an important global problem to be studied since many people that have cancer have a weakened immune system, increasing their susceptibility to contracting COVID-19 and potentially dying.
We need to better understand how COVID-19 impacts cancer patients because they are more vulnerable to infections than the general population. One previous study found that people with cancer have a higher probability of serious events compared to those without cancer, such as death, ICU admission, severe symptoms, and need of mechanical ventilator. However, they only studied a small number of patients, so a larger study was necessary.
Researchers from Hubei, China conducted the first large cohort study of cancer patients to ask whether they are more vulnerable to SARS-CoV-2 than those without cancer. The study team enrolled 105 hospitalized patients with cancer and COVID-19 and 536 hospitalized non-cancer patients with COVID-19.
For each participant, researchers documented their cancer type and stages. This helped researchers determine which stage of cancer makes patients more prone to severe COVID-19. They also documented which patients required invasive ventilation or ICU stays, which patients had severe symptoms, and which patients died. The scientists were also interested in the effects of cancer treatment on COVID-19 outcomes. They compared the rates of death for patients receiving either radiotherapy, chemotherapy, surgery, targeted therapy, or immunotherapy.
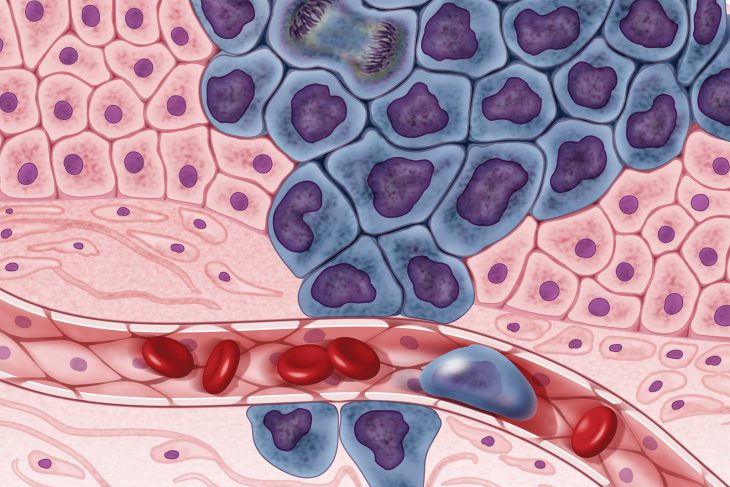
The researchers expected that people with cancer would be more vulnerable because certain cancer treatments weaken the immune system or lead to poor nutrition. Some cancer types can even alter the function of the immune system’s many infection-fighting cells.
They found that cancer patients who contract COVID-19 tended to have more severe symptoms and were more likely to die from complications of the infection. Of the non-cancer patients, 5% died, 7% were in ICU admission, 18% had critical symptoms and 0-1% had required ventilation. For patients with cancer, 11% died, 19% needed ICU admission, 35% had severe symptoms, and 10% required ventilation.
In the general population, 2-3% of COVID-19 patients will die from the disease. However, cancer patients with COVID-19 had a higher death rate. For example, patients with metastatic cancer, or cancer that has spread beyond its onset location, had a 23% death rate compared to non-cancer or non-metastatic cancer patients, who suffered a 4-5% death rate. Severe symptoms of COVID-19 were found to be most common in patients with stage IV hematologic (blood) cancer, lung cancer, or metastatic cancer of any type.
The authors say that patients with hematologic malignancy, or cancer of the blood tissues, had a higher mortality rate. This makes sense since the immune system operates largely in the blood. Since COVID-19 is a respiratory disease, patients with lung cancer had the second-highest risk levels of mortality rate, ICU admission rate, and severe critical symptoms. Patients with non-metastatic cancer, on the other hand, did not die any more often than those without cancer.
In general, patients with cancer experience more difficult outcomes than those who are cancer free, particularly if their cancer was advanced or in organ systems that are also affected by COVID-19.