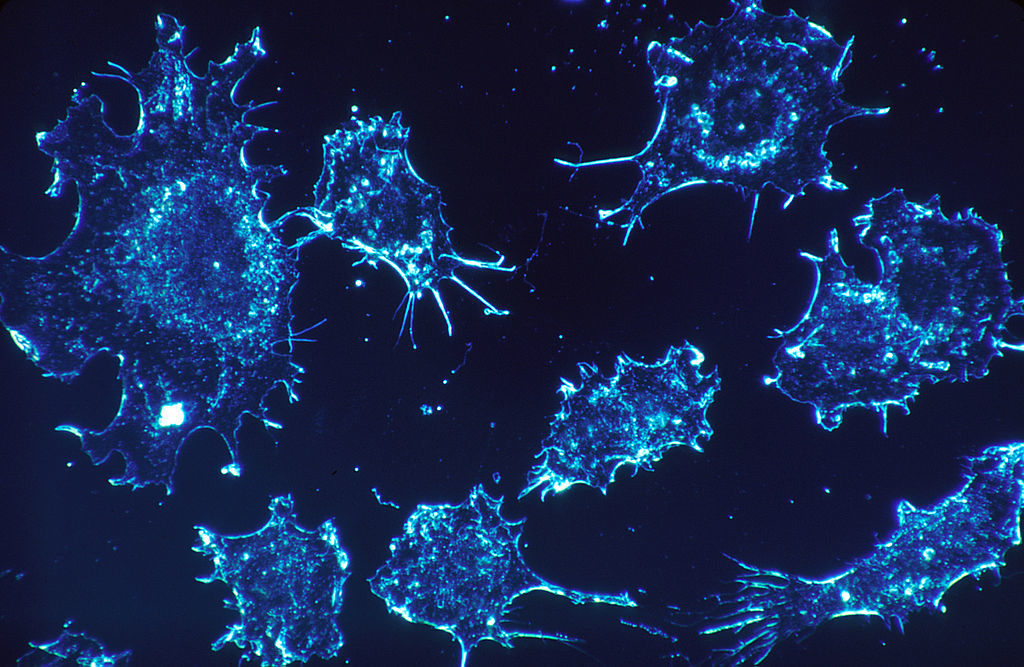
Tens of thousands of individuals suffer from a form of cancer known as chronic myeloid leukemia. To combat this specific cancer, many patients take chemotherapy drugs with successful results. Chronic myeloid leukemia is often treated with a class of chemotherapy drugs called tyrosine kinase inhibitors. Tyrosine kinases are enzymes that can speed up a human cell’s growth or division, which can lead to cancer when it gets out of control. The specific tyrosine kinase that causes chronic myeloid leukemia is called the BCR-ABL enzyme. When this enzyme is inhibited or blocked, it can slow down or stop the out of control cell growth seen in chronic myeloid leukemia.
Two popular examples of chronic myeloid leukemia chemotherapy drugs include nilotinib, commonly known as Tasigna, and imatinib, commonly known as Gleevec. In a recent clinical trial, the effects of these medications were compared after five and ten years of consistently taking a specific dosage of medication, which is called medication adherence. Two hundred eighty-two patients were instructed to take 300 mg of nilotinib twice daily, 281 took nilotinib at 400 mg twice daily, and 283 took imatinib at 400 mg once daily. Some patients dropped out of the trial prematurely due to personal or medical reasons, which is typical for any clinical trial.
The researchers used several factors to judge the success of the drugs, including how much cell growth enzyme was found, known as the molecular response rate, and how many cancer cells survived. Other aspects they measured were how fast the disease progressed, overall survival rate, chance of cardiovascular events, and the possibility for remission without the need to continue treatment. Cardiovascular events are occurrences where the heart muscle is damaged, for example, a heart attack. Remission is when a person suffers from fewer symptoms of chronic myeloid leukemia and can be partial or complete.
After five years of medication adherence, 50-60% of the patients remained in the study in each dosage group. The molecular response rates were higher in patients who were taking nilotinib. A high molecular response rate is a good sign because this means more of the cancer cells have disappeared or died due to treatment. Patients on either dose of nilotinib were less than half as likely to progress to more aggressive chronic myeloid leukemia, compared to those on imatinib. Also, there was a better chance for a more successful remission without continuing treatment while on nilotinib.
After ten years of medication adherence, 30-35% of the patients remained in the study in each dosage group. Similar to what was seen after five years, the molecular response rates were higher, fewer patients progressed to more aggressive forms of chronic myeloid leukemia, and also patients had a better chance for remission without treatment when on nilotinib.
The nilotinib group did have a higher rate of cardiovascular events, which was the medication’s only downside. In the group of patients who were taking 300 mg of nilotinib twice-daily, 46 cardiovascular events occurred. Sixty-five cardiovascular events occurred for patients on 400 mg of nilotinib twice-daily. Ten cardiovascular events occurred in the once-daily 400 mg imatinib group. These totals are after the full ten years.
The three groups had similar survival rates. For nilotinib, survival was 88% at 300 mg and 90% at 400 mg. The overall survival rate for the imatinib was 88%. When comparing the effects of each medication, researchers concluded that patients who took nilotinab experienced fewer side effects than with imatinib.
This study can help chronic myeloid leukemia patients and doctors decide which medication, imatinib or nilotinib, would be a more safe and effective choice. The authors also warn patients and doctors of possible side effects, which could be important if the patient is not in good cardiovascular health. Nilotinib is generally the better choice when compared to imatinib according to these findings. A continuation to this study can be done to see if any other medications have the same beneficial results as nilotinib, with a lower number of cardiovascular events. Another continuation study can be to test whether imatinib and nilotinib’s negative effects will change based on the sex of a patient.