Two patients with chronic leukemia achieved remission in 2010 after being injected with a genetically modified version of their immune system’s own T cells, called CAR T cells. Over a decade later, these patients have remained in remission because of these long-lasting cells. These were the first patients treated with this therapy to sustain remission 10 years after treatment, which marks a huge step in treatment and understanding of leukemia. CAR T cell therapy is only the second form of gene therapy approved in the United States.
CAR T cells are genetically engineered T cells, which are white blood cells that fight infected cells. Normally, T cells have T cell receptors on their surface that can recognize pieces of pathogens that are infecting the patient’s cells. This function allows T cells to recognize infected cells and take part in the body’s defense system.
Unfortunately, the reason why T cells alone cannot fight cancer is because the T cells only recognize strange proteins. They are unable to recognize cancer as a “foreign molecule” because it comes from the body’s own tissue. CAR T cells are different – they are armed with a special receptor that lets them “see” cancer.
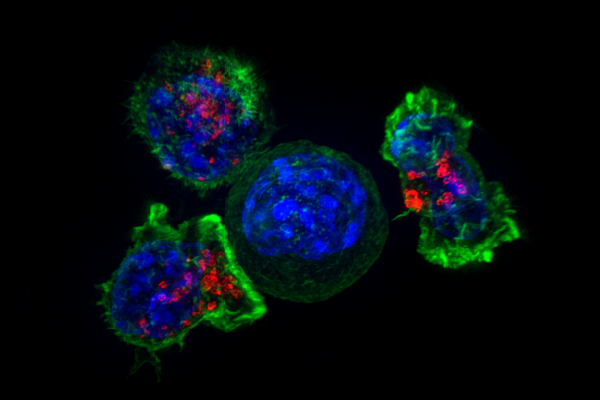
In CAR T cell therapy, T cells are first collected from a patient’s blood. In the lab, a virus is used to produce molecules called CARs, or chimeric antigen receptors. These CARs recognize molecules displayed on the cancer cells, telling them apart from pathogen-infected cells. The patient’s T cells are genetically modified to make CARs using the virus. After modification, the CAR T-cells are injected back into the patients. These T cells, once modified with CARs, are capable of specifically targeting tumors and killing cancer cells.
Little did these patients know that following this treatment would put their end stage leukemia into remission the same year of treatment. The persistence of T cells against chronic lymphocytic leukemia, the most common type, in these patients is the longest known to date. Despite the successes of 2010, however, scientists still don’t know much about how CAR T cells affect the body in the very long term, such as beyond 10 years. The research team conducted a more recent study to find out.
There are two types of T cells within the body that are relevant to these patients: CD4+ helper T cells and CD8+ killer T cells. The helper T cells function to help other immune cells have the ability to “see” invading cells. Meanwhile, the killer T cells are able to kill the invading cells directly. After drawing blood from the two patients, they found that both had a distinct population of highly activated helper T cells that developed as a result of dominating the original killer T cell population. Thus, the original killer T cells had turned into helper T cells with both abilities: killing invading cells and helping other immune cells “see” invading cells.
To detect or find the T cells present in each patient, scientists used a method called flow cytometry that allowed them to map and detect where in the body the CAR T cells reside years after injection. Also, they used a method called single cell profiling to look at the DNA sequences of the CAR T cells to understand the characteristics of the long lasting T cells to show that these cells have characteristics of killing and targeting cancer cells.
Researchers found that there are two phases of the CAR T cells, the first phase containing “CD8+” or killer T cells that can kill cancer cells or virus infected cells, and the second phase containing “CD4+” helper T cells with characteristics of both killer T cells and helper T cells. The first patient still had functional CAR T cells present after 9 years, which was a key component in achieving remission. The second patient had CAR T cells present 7.2 years after the initial infusion.
These findings offer a deeper understanding of what happens in the years following CAR T cell treatment. Overall, the results of this study support the effectiveness of CAR T cell therapy for leukemia. The researchers recommend more research to test T cells in other blood cancers such as lymphomas or even solid tumor cancers. A considerable amount of research is still needed to test this form of therapy for other cancer and diseases in the future.