You’re out for a run on your favorite trail, and you hear something rustle in the bushes. You immediately jump to attention, eyeing a snake. Your body’s automatic reaction to the snake can be attributed to your amygdala.
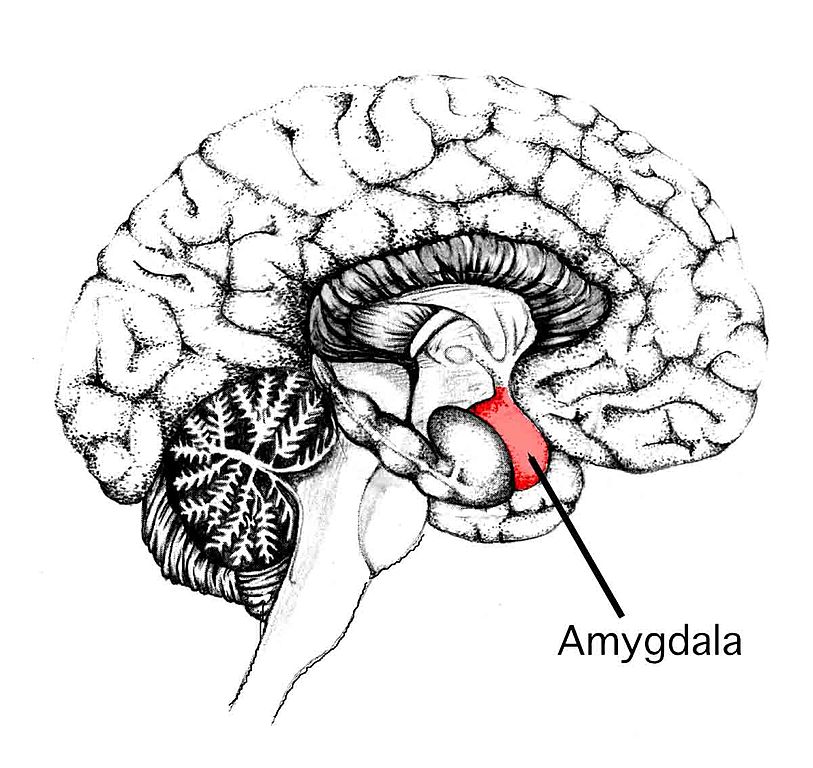
The amygdala is a region of the brain where our fear response takes place. For example, if we need to run from a dangerous threat, this part of the brain tells our bodies to take action. This is known widely as the fight or flight response. In prey animals, such as mice, this response also includes “freezing” behavior, where the animal spends a longer time than usual in a crouching position and experiences changes in its blood pressure.
Anxiety is a type of chronic low-level fear that is also associated with the amygdala. Anxiety disorders are common, affecting approximately 18% of the population of the United States and are usually treated with medication, therapy, or some combination of the two. Understanding how the brain and the rest of the body interact is critical for informing potential treatments.
Previous research suggests that the digestive system and the brain affect one another, at times in undesirable ways. A groundbreaking study in the journal Molecular Psychiatry explored a particularly fascinating aspect of the brain-gut connection – the influence of intestinal bacteria on the function of the amygdala.
It can be difficult to imagine how two organs that are so far away from each other in the body can be so intimately related. The study does not necessarily provide a mechanism for how bacteria affect the brain, but it does show a relationship between the presence of gut bacteria and changes in the fear response in mice. These early results can be used to inform future research in both test tubes and in living humans.
Researchers at the Science Foundation Ireland-funded APC Microbiome Institute at University College Cork in Ireland set up their experiment using a specially bred variety of research mice called Germ Free mice. These mice have sterile digestive systems, meaning they have no bacteria in their intestines. The digestive tract is typically populated with a mixture of bacteria, so these mice are unique.
Researchers began with one group of germ free mice and one group of ordinary mice. When the germ free mice were 21 days old, half of the germ free mice were sent to live with the ordinary mice in order to acquire their gut bacteria. The study refers to these mice as ex-germ free. After allowing the ex-germ free and ordinary mice to interact, they exposed all three groups of mice to a sound held for 30 seconds, followed by a light shock at the bottom of the cage during the last 2 seconds of the sound. The purpose of this was to train the mice to associate the electric shock with the sound. In the future, the mice will fear the sound even when the shock is absent. This is called conditioning and it happens to humans, as well.
After training the mice to associate the sound with the shock, the researchers waited 6 hours. Then, they exposed all three groups of mice to the sound without the shock. The researchers then observed the behavior of the different groups of mice, looking for indications of a fear response, such as freezing.
The germ free mice displayed less freezing behavior in response to the sound compared to the conventional mice and the ex-germ free mice. The conventional and ex-germ free mice showed similar fear responses. According to these observations, the absence or presence of gut bacteria has an affect on the action of the brain’s fear center.
In order to learn about what was going on in the bodies of the mice, researchers used two techniques called high-throughput sequencing and microarray analysis. These techniques allowed the researchers to examine how the physiology of the brain changed in mice who were conditioned to fear the tone and mice who were never exposed to the fear training at all (referred to in the study as “naive”). These techniques allow researchers to see which genes in the body are activated, or expressed, and which are not, giving insight into how the cells responded.
The fear-conditioned germ-free mice and the naive germ-free mice showed completely different sets of genes activated in the amygdala. Moreover, the genetics data acquired suggested that the germ-free mice had hyperactive amygdala compared to ordinary mice.
These results may seem contradictory. One might expect that mice showing a lower fear response would have an under-active amygdala. However, the results of this study likely indicate that the poor memory of the sound stimulus might lead to poor memory of what is to be feared and what isn’t. The researchers’ conclusions suggest that in order to have a “normal” fear response, the intestines must have a healthy mixture of bacteria. So far, most of the data on this subject is in mice, but it is an exciting and unfolding field of study that may inform new treatments for anxiety disorders.