The challenge with treating cancer is finding the best treatment plan for individual patients. Some patients have a strong response to a certain treatment while others may not. In a new study, scientists set out to identify what factors would predict a full recovery in patients that were diagnosed with melanoma and then treated with talimogene laherparepvec. This knowledge would allow for the best treatment to be chosen for each patient.
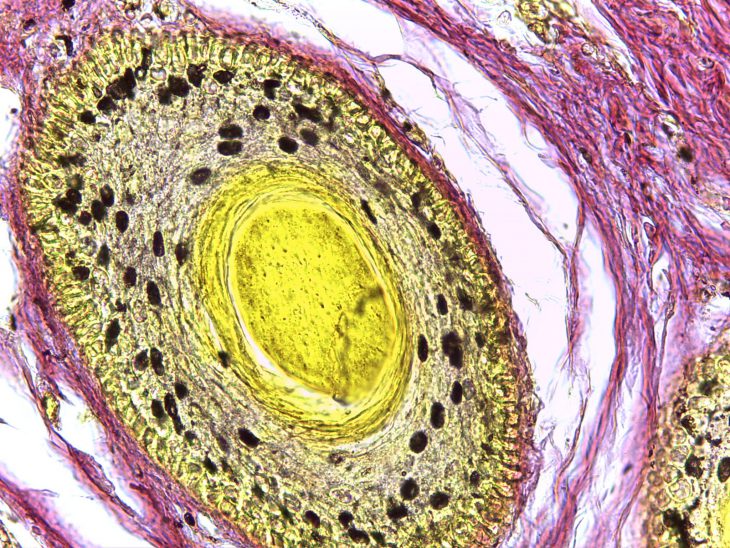
In December 2021, the Food and Drug Administration approved talimogene laherparepvec to treat melanoma using a modified herpes simplex type 1 virus. This virus is commonly known as “herpes” and can cause contagious sores on the mouth and genitals. However, in this case, the virus has been modified to not cause sores and instead to treat cancer. The new treatment works in two ways. First, the virus infects the tumor cells, replicates inside them, and then kills them by bursting the cells open. The second way the treatment works is by activating the immune system to kill the tumor cells.
Usually herpes infects both skin cells and cells that make up the sensory system. Scientists have removed a particular gene from this herpes virus so that it will no longer be able to infect the sensory cells. Melanoma is a cancer of the skin, so by removing this gene, the modified virus is able to just infect the skin cancer cells.
Researchers selected patients at the Netherlands Cancer Institute from 2017 to 2020 to receive the treatment. Staff administered the treatment by injecting the modified virus every two weeks directly into tumors or into the lymph nodes. Therefore, the tumor had to be in a location that could easily be reached with a needle. Researchers collected data on each patient including sex and location of the tumor. Scientists observed how the tumors responded to the treatment and recorded any negative side effects. They determined the level of response by visual inspection of the size and number of tumors, and by a CT scan every three months.
After treatment, 79% of patients had smaller tumors. Sixty-two percent of patients had a complete response, meaning their tumors disappeared, including those whose tumors eventually returned. Fifty-one percent of patients were cancer-free for more than six months. Most patients had flu-like symptoms after the treatment, but only one out of 93 patients had a serious side effect. That patient recovered and continued treatment with no further complications.
Researchers completed two important goals in this study. The first was to determine what variables are associated with a complete response to the treatment, meaning all their cancer was gone, at least temporarily. Researchers used mathematical analysis to determine what variables were associated with a complete response. Many of the factors were related to metastasis, which is when cancer cells spread to other parts of the body. The data showed that patients with smaller metastases, tumors that were on the skin as opposed to under the skin or in lymph nodes, and patients who did not receive previous treatments were more likely to have a complete response.
The second goal they completed was to create a formula to predict how well a patient would respond to the treatment. The model included three things: the number of metastases, the location (skin, under the skin or lymph node), and the diameter of the largest tumor. Researchers were able to provide a quick and easy visual way for doctors to predict their patients’ outcome and determine if this treatment is the best option.
This group of patients showed the highest response rate to treatment with talimogene laherparepvec to date. However, this study only used data from one clinical center and a small number of patients. This study should be repeated with more patients and different clinical centers to further support their findings. Their results show that the new treatment is most effective with small tumors. Currently doctors use surgery to remove small tumors that have spread, but these results show that this new treatment could be a better option in this scenario. These same authors have now started a clinical trial to address the weaknesses of this study and confirm the new treatment’s effectiveness.