Would you let a scientist implant a parasite in your brain to treat an illness? The idea of using a parasite as a medical tool might seem outlandish, but it also offers hope for conditions like Parkinsons and Alzheimer’s. Researchers have speculated that if a parasite could deliver drugs directly to the brain, it might help doctors treat these conditions.
An international team of scientists is doing just that. They are using a single-celled parasite known as Toxoplasma gondii, which causes an infection called toxoplasmosis. The parasite naturally travels from the human gut to the central nervous system and delivers proteins to host cells. In the experiment, bioengineers hacked systems within the T. gondii’s cells that produce and release proteins outside the cell, called secretion systems.
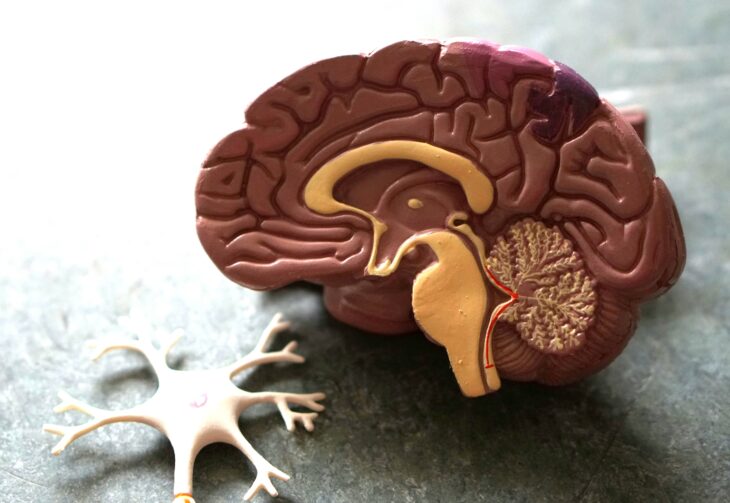
The team explained that getting drugs to the brain is difficult because the blood-brain barrier shields the brain from potentially harmful substances. T. gondii has evolved the ability to cross the blood-brain barrier, so it could help with this process. First, they tested a protocol using T. gondii to cross the blood-brain barrier in mice to see if it could be used in humans. After that, they did trials in human brain cells, called neurons. Lastly, they applied the human brain cell results to the fully intact brains of mice to see if they could potentially be applied to a full human brain.
Their T. gondii-mediated drug delivery system involved a protein made up of at least 2 regions from different genes that are joined together so that they are transcribed and translated into a single unit. This type of system is called a protein fusion. In particular, they combined therapeutic drugs with a T. gondii protein called taxifolin to deliver the drugs into the brain.
At first, the scientists had difficulty determining how much to dilute the medicinal compound in the solution, called its dilution factor. They explained that the concentration had to be low enough for the proteins to pass through the blood-brain barrier but high enough to be therapeutically effective. They used trial and error to determine the right dilution factor to successfully deliver the therapies to the right brain location.
The next step was to deliver the therapeutic proteins into brain cells using T. gondii. The researchers used mouse brain cells grown in the lab and a specific protein that controls the movement of molecules across the brain cell membranes, called a vesicular transport protein. They demonstrated that the modified T. gondii carried the healing proteins and successfully delivered them to lab-grown mouse brain cells.
Next, the researchers tested the therapeutic process on human brain cells grown outside a living organism. They demonstrated that the T. gondii-delivered therapeutic proteins could bind to DNA in the lab-grown human brain cells. Once bound, they found that the therapeutic protein altered gene expression in the lab-grown brain cells.
Lastly, the engineers showed that this therapy could be successful using whole mouse brains. While the mice were alive, the researchers ensured that the therapeutic protein had successfully passed the blood-brain barrier. Then, they euthanized the mice painlessly and examined their brains. The researchers used 3D imaging to light up specific neural pathways and markers in the mice’s brains. They confirmed that the engineered proteins carried the therapeutic protein into the brain intact.
The researchers concluded that their results mark progress in delivering medicine through engineered parasites, but additional investigations are required to determine the method’s possible advantages and drawbacks. Based on the success of this study, they suggested that using engineered parasites for drug delivery could offer new treatment options for brain-related diseases.