A recent study has highlighted a link between the appendix and Parkinson’s disease. This is interesting because Parkinson’s disease is well known as a neurodegenerative disorder – disorders in which brain cells, or neurons, die off as the illness develops. As a result, one might not expect to see a link between the appendix, located at the beginning of the large intestine, and a disease like Parkinson’s which occurs primarily in the brain. However, thorough analysis of large amounts of data tracking individuals over 5 decades, the researchers of this study found that removal of the appendix was indicative of a lower risk of developing Parkinson’s disease. The risk was actually 19% lower in individuals who had their appendix removed. In addition, individuals that did develop Parkinsons disease did so at a later age (disease onset was on average 3.6 years later).
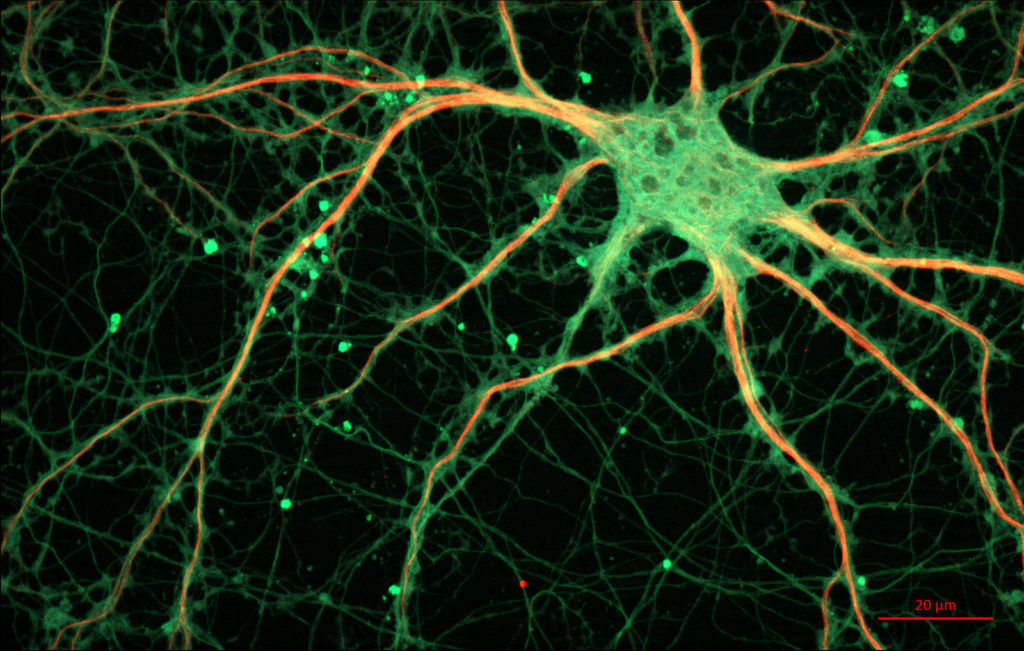
What is important is that this research actually fits in well with an emerging understanding of Parkinson’s disease wherein the role of areas outside of the brain are becoming increasingly implicated. Much research in recent years has focused on the role of the digestive system or “gastrointestinal system” in the disease. In fact, our gastrointestinal tracts (pictured on the left) actually contain many neurons which are responsible for the unconscious control of our digestive function. For example, functions such as the movement of food waste through the intestines are controlled by such neurons. These neurons, collectively known as the enteric nervous system, are so abundant that they are often referred to as a “second brain”. Something that may be surprising is that these neurons in the enteric nervous system have actually been reported to contain well known Parkinson’s disease indicators during the early stages of the disease.
These disease indicators are misfolded “alpha-synuclein” and “Lewy bodies”, which are actually closely related. Lewy bodies are clumps of protein that are seen in the neurons of Parkinson’s patients, and a major part of what forms Lewy bodies is the protein known as “alpha-synuclein”. Alpha synuclein is an extremely abundant, naturally occurring protein in the brain. In normal healthy brains, alpha synuclein is suggested to have many important roles, including in normal brain cell signalling. However, in Parkinson’s, a mistake occurs in the folding of the protein alpha-synuclein. This mistake in folding makes it more likely to clump together. These indicators have long been seen in neurons in the brain of Parkinson’s patients, and it is significant that they are now also found in the enteric nervous system of the digestive system. Much of the research into Parkinson’s has centered on alpha-synuclein. Many therapies in development now are attempting to stop it from clumping together, as well as clear existing clumps.
The researchers of the study then analysed appendix tissue from people who had undergone routine appendectomies, where they found high levels of alpha-synuclein contained within the appendix. Interestingly, this was found in both healthy individuals as well as in patients with Parkinson’s disease, however the alpha-synuclein was present in significantly higher levels in disease patient appendixes. They also found through biochemical experiments that this appendix tissue itself was able to cause a clumping together of alpha-synuclein in a manner resembling what occurs in Parkinson’s disease. This finding fits in well with previous research that found misfolded alpha-synuclein is able to spread somewhat like a virus, where it can move from cell to cell and cause the formation of more alpha-synuclein clumps and Lewy bodies in neurons. The researchers suggest that this finding of alpha-synuclein in the appendix may mean that misfolded alpha-synuclein can travel from the appendix to the brain as one of the potential mechanisms that leads to Parkinson’s disease. Now, a clearer model of Parkinson’s is emerging in which the digestive system, appendix, and brain are all important aspects of what contributes to the disease. Hopefully, a better understanding of all the factors involved will lead to better disease diagnosis and treatment in the future.
Appendix image caption: Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. [CC BY 3.0], from Wikimedia Commons