Each year, roughly 600,000 women are diagnosed with new cases of cervical cancer, accompanied by 350,000 deaths worldwide. In the United States alone, The American Cancer Society estimates that in 2022, 14,000 new cases will arise as well as 4,280 deaths. If this disease is detected early, it is not very invasive and can be treated with surgical removal of the uterus and lymph nodes. Those who have more enduring or recurrent cases require platinum-based chemotherapy, which can only be given in limited doses due to severe side effects. Most patients’ cancers progress beyond this treatment, leaving them with limited treatment options.
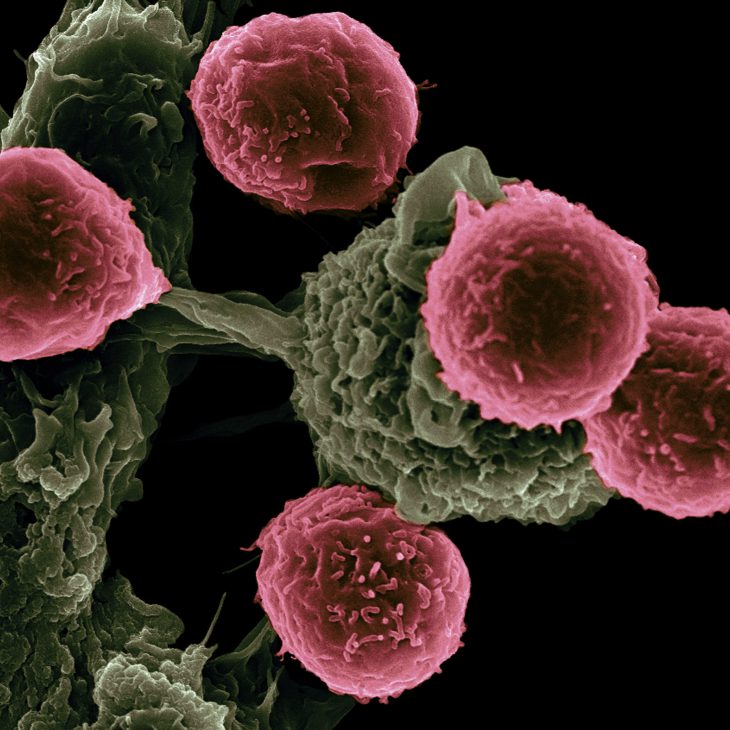
Immunotherapy is becoming an increasingly popular method to treat many different cancers, as it stimulates the immune system and improves the body’s natural ability to fight off these cancers. Cancer cells produce proteins that stop the body’s immune system from attacking them. Some immunotherapies are checkpoint inhibitors, which block these proteins, allowing the immune system to work properly again.
Many healthy body cells need these proteins so that the immune system doesn’t attack them. But when healthy cells become cancerous, these proteins become a problem. PD-L1 is one such protein. It stands for “programmed death ligand 1” and it protrudes from the surface of cancer cells and keeps immune cells from attacking them. Many cancers have high levels of PD-L1, allowing them to avoid being killed by the immune system.
In order to combat this, researchers have developed PD-L1 blocking antibody treatments. Two of these are cemiplimab, a drug often used to treat skin and lung cancers, and pembrolizumab, which is currently the only anti-PD-L1 agent approved for use in the United States as a second option treatment for patients with recurrent or metastatic cervical cancer. Unfortunately, pembrolizumab does not work for patients whose cancers do not produce PD-L1, or whose proportion of PD-L1 positive cells over normal tumor cells is less than 1. A score of less than 1, or less than a one-to-one ratio, means that less than half of the tumor cells produce PD-L1. This ratio is called the combined positive score, or CPS for short.
From July 2017 through August of 2020, a clinical trial was conducted with patients with recurrent or metastatic cervical cancer who had previously undergone platinum-based chemotherapy to see if there was any significant difference in the lifespan of those treated with cemiplimab vs those treated with the investigator’s choice of a different chemotherapy. Six hundred and eight women (ages 22-87) were deemed eligible to participate if their cervical tumors progressed after receiving platinum-based chemotherapy. The patients were randomly and evenly split up into two groups to undergo the different treatment options.
The researchers found that treatment with cemiplimab resulted in 31% lower risk of death in those with basal-cell carcinoma and 27% lower risk of death in those cases with squamous-cell carcinoma compared to other treatments. However, it was unclear if cemiplimab had an effect on the patient’s survival without the cancer getting worse. A small outlying group of cemiplimab patients did seem to benefit, but overall the effect was similar between the two treatment groups.
In many cancers, a scale of 1 to 5 is used to grade how fast cancer cells are growing, where 5 is the most aggressive. Although cemiplimab treatment took longer than chemotherapy (15.2 weeks vs 10.1 weeks), patients with any grade of cancer treated with cemiplimab saw fewer adverse effects, especially in grade 3 and higher.
Interestingly, researchers also found that cemiplimab also worked on patients whose tumors were PD-L1 negative or had a CPS of less than 1. This is important, as this treatment may benefit many women whose cancer does not express the checkpoint inhibitor and thus will not see results from the drug that blocks them – pembrolizumab. These findings suggest the use of cemiplimab to treat recurrent or metastatic cervical cancer may be beneficial to some women who previously received platinum-based chemotherapies.